Cost-effective medical technologies for supporting infection management
Antimicrobial Resistance (AMR) is a major global public health threat, with the potential to take us back to a ‘pre-antibiotic era’, where patients could die from simple infections and life-saving care can no longer be delivered safely. The cost of treating complications due to resistant infections can exceed USD 28.9 billion every year across 34 OECD and EU/EEA countries 1. This adds to the burden of Healthcare-Associated Infections (HAIs), which is estimated to cost €7 billion in Europe 2.
Moreover:
- One in five bacterial infections are resistant to antibiotic treatment in OECD countries.
- Resistant infections claim the lives of around 79 000 people every year across these countries. The elderly bear the brunt of the AMR death toll, with around two out of three deaths due to AMR occurring among people above 65 years of age.
- Healthcare-associated resistant infections account for more than 60% of AMR-related deaths. 1
These challenges add extra strain to our already overburdened healthcare systems, risking their economic sustainability.
Addressing AMR & HAIs offers a compelling return on investment with a net return of 5 to 13 dollars for every dollar invested, depending on the specific interventions 1 3.
As AMR continues to reduce our ability to effectively manage infections, we need to invest not only in technologies to control and prevent infection, but also in evidence and education to understand which packages of care offer the best approach for each patient based on a holistic risk assessment.
The impact of utilising medical technologies to reduce healthcare costs and productivity losses associated with AMR & HAIs
Medical technologies (medical devices and in vitro diagnostics) contribute to preventing and controlling AMR and HAIs, resulting in cost efficiencies in four distinct ways, illustrated below:
-
Preventing and containing healthcare-associated infections and the development and spread of resistant bacteria in healthcare settings to manage antimicrobial resistance. Earlier interventions can often avert more costly advanced care, enabling more efficient resource use.
-
Supporting appropriate therapy by detecting and identifying bacterial infections and their susceptibility to antibiotics, improving patient care and outcomes thus saving costs globally, for now and future generations.
-
Monitoring and tracking resistance and enabling patient compliance to the appropriate use of antibiotics. Early warnings avoid unnecessary costs.
-
Outbreak management and surveillance to track, contain, and prevent the spread of pathogens at all levels, from the hospital to international levels. Preparedness is a sound investment.
Interactive Patient Pathway Timeline

Before admission to the hospital / in the community
The largest proportion of antibiotic consumption in humans takes place in the community (more than 90 % in Europe 4). It is therefore essential that the appropriate use of antibiotics is addressed first in the community setting, to ensure new and existing antibiotics remain effective for as long as possible. For patients undergoing either an elective procedure or an emergency admission in a hospital setting, protocols should be in place to help reduce the risks of HAIs, and the development of resistance. Some non-pharmaceutical interventions have emerged as highly cost-effective when incorporated into a protocol that includes a full risk assessment. Decolonisation using e.g. topical agents, diagnostics, and isolation via contact precaution have been popular approaches to infection control, often surpassing standard care in costs and efficiency 5.
What can be done by technology?
Technology examples:

Arrival at the hospital
Prompt clinical assessment supported by rapid diagnostic testing for infectious diseases can inform optimum patient management, avoiding unnecessary admission or preventing missed admission and enabling timely isolation decisions. Such an enhanced patient flow reduces pressure on hospital resources, personnel and costs.
What can be done by technology?
Technology examples:

In the operating room
An infection can occur after surgery in the part of the body where the procedure took place. These are called surgical site infections (SSIs) and account for more than 50% of all adverse events in hospitals 14. Most surgical wound infections are acquired in the operating room from the patient’s own microbial flora. The remainder are acquired mainly from the staff in the operating room during surgery 15. It is estimated that half of all SSIs are preventable 16. Preventing SSIs is not only beneficial for the patient but could also provide a source of cost savings for the hospital. To reduce the probability of an SSI, basic protocols which include hand decontamination, sterile drapes and gowns, gloves – preferably double gloving to avoid risk of perforation – and antiseptic skin preparation should all be utilised.
What can be done by technology?
Technology examples:
During hospital stay and recovery
Patients staying at a hospital expect to recover quickly and receive the best possible care without being exposed to any unnecessary harm. Developing a resistant infection can prolong hospital stay, impede quick recovery, and increase healthcare costs. Appropriate use of medical devices and in vitro diagnostics can help avoid unnecessary and costly therapies, reduce exposure to antibiotics, resulting in more predictable patient pathways, reduced length of stay, and lower probability of re-admissions.
What can be done by technology?
Technology examples:

Discharged and back at home
There is an increasing trend towards outpatient clinics and day surgery, meaning that patients continue to be treated in other healthcare facilities or in their home environment, thereby reducing the demand on healthcare resources.
What can be done by technology?
Technology examples:
Pre-surgical nasal screening
These technologies can be used to detect whether a patient is carrying a certain type of bacteria. Advanced screening technologies can provide sophisticated and rapid test findings before (e.g. during the pre-admission consultation) or on admission. This can help to reduce infection rates in patients during the medical intervention and facilitate the appropriate use of antibiotics while avoiding contaminating other patients and staff.

Point of Care C-Reactive Protein (CRP) test
In high-income countries (HICs), 8 of 16 scenarios evaluating Point Of Care Testing (POCT) for respiratory tract infections were found to be cost-effective at the threshold of £33.80 per prescription avoided 6. More specifically, the use of C-reactive protein (CRP) point-of-care tests has been shown to significantly reduce antibiotic prescriptions for lower respiratory tract infections, without compromising either patients’ recovery or satisfaction with care 7.

Streptococcus A pharyngitis test
Acute pharyngitis is a frequent cause of visits and antibiotic prescriptions in primary healthcare facilities 8. Although Streptococcus A is the cause of only 15% to 30% of cases, antibiotics are prescribed in 55% to 75% of cases 8. Rapid testing for Streptococcus A enables healthcare providers to accurately diagnose the cause of pharyngitis, thereby guiding the targeted use of antibiotics in any healthcare setting. According to a NICE Evidence Review, a significant reduction in initial antibiotic prescribing using Streptococcus A POCT has been found in 2 studies 9.

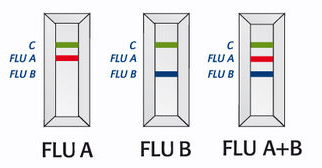
Influenza A and B viruses in human nasopharyngeal specimens
Influenza (commonly known as flu) is a highly contagious acute infection of the respiratory tract. Types A and B are the most common types of human influenza virus. They can circulate simultaneously, but usually one type is dominant during a seasonal epidemic. Although a flu infection is not normally severe, certain populations are at higher risk of developing complications. Rapid and accurate diagnosis means reducing the risk of transmission and outbreak, preventing inappropriate antibiotic use, and ensuring the early prescription of antiviral medication for high-risk patients.
Patient screening for multi-drug resistant organisms
Screening tests, such as chromogenic culture media, are ready-to-use tools for the selective isolation, enumeration, and identification of bacteria in 18-24 hours. They deliver more reliable differentiation of pathogens and multi-drug resistant organisms, faster and easier reading of results, and enhanced performance compared to traditional culture media.
A cost model found that targeted screening of at-risk patients at admission, combined with dedicated staff for identified carriers of Carbapenemase-producing Enterobacterales (CPE), was the most cost-effective intervention to control the spread of CPE 10. It justified €17,407 per avoided CPE case, with a reduction of 64% CPE acquisition.

Patient isolation
Influenza-positive patients are 1.55 times more likely to be appropriately assigned to isolation facilities when tested with a rapid multiplex PCR test for respiratory viruses. This is an important tool for preventing nosocomial transmission, which can be costly for hospitals 11.

Better management of children presenting with meningitis or encephalitis
Patients with positive viral detection by multiplex PCR have had fewer days of antibiotic therapy, fewer days of antivirals, and reduced length of stay 12 13. This can translate to 31% lower median hospitalisation costs (€1,042 compared to €1,522), resulting in €22,834 in yearly savings, as well as reduced anxiety for the patient and their family.
Screening for Carbapenemase-producing bacteria
These tests give reliable results in 30 minutes to 2 hours, making it a quick and easy way to control Carbapenemase producers while meeting diagnostic and screening challenges, improving patient management and controlling HAIs. The rapid detection time ensures that appropriate therapy and patient isolation measures are implemented.

PCT - Early diagnosis and monitoring
Procalcitonin (PCT) helps differentiate bacterial from viral infections, and the early detection of an elevated PCT level in patients with suspected bacterial infections enables earlier antibiotic treatment. PCT also supports informed decisions on when to continue or discontinue antibiotics, thereby improving patient care and reducing antibiotic misuse, which helps control the emergence of antimicrobial resistance.

Rapid pathogen identification
Rapid identification of the pathogen causing an infection is crucial for guiding diagnosis and antibiotic therapy. Innovative technologies, such as multiplex PCR systems, can identify a wide variety of bacterial, fungal, viral, and parasitic pathogens that cause respiratory, bloodstream, gastrointestinal, and meningitis infections, as well as antibiotic resistance genes, in just one hour. This enables the quick prescription of antibiotics and helps avoid misuse.

Cleaning and disinfection procedures
These procedures are essential for reducing the number of microbes in the area near the patient. It is also crucial to put in place personal protective barriers (e.g., gloves, gowns) to prevent healthcare workers from transferring bacteria to other patients.

Catheters and closed IV systems
Substantial reductions in catheter-related bloodstream infections can be achieved with the aid of advanced medical technologies, along with complementary improvements in practices. These include integrated safety catheter systems and closed IV access, alongside associated care and maintenance.

Antimicrobial dressings
Catheter-related bloodstream infections (CRBSIs) incur an annual cost of €271 million to European healthcare systems. Substantial reductions in CRBSIs have been achieved with the aid of antiseptic-impregnated antimicrobial catheter dressings.

Antibacterial sutures
Evidence supports the case for adopting antimicrobial sutures as part of a comprehensive bundle of care to prevent surgical site infections in individuals who require wound closure following a surgical procedure. Cost modelling shows that antimicrobial sutures are cost-saving compared with standard absorbable sutures by an average of £13.62 per patient 17. These savings stem from a reduction in surgical site infections.

Active patient warming
Hypothermia can occur as an adverse effect of surgical procedures and is a significant risk factor for developing Surgical Site Infections (SSIs), cardiac events, and the need for blood transfusions. The use of active patient warming techniques during the procedure is proven to significantly reduce the rate of these infections from developing. Furthermore, a medium cost saving of 16% per patient can be achieved, compared to the non-use of devices. Moreover, the social productivity cost is reduced by around 30% and the overall number of hospital days is reduced by between 15% and 26% 18.

Impregnated incise drapes
The antiseptic contained in the drape is continuously released onto the skin during the procedure, preventing bacteria from contaminating the wound during the operation. These drapes prove to be cost-saving, as illustrated by the avoidance of 773 000 € for a series of 5100 consecutive cardiac surgery patients 19, due to the lower incidence of surgical site infections (SSIs) and consequently the avoidance of complication treatments.

Rapid identification of bloodstream infection pathogens
Studies and cost models show that rapid diagnostics testing, associated with the prudent use of antibiotics, not only improves the quality of care but also generates cost savings of up to $27,537 per patient20 – a win-win case for all stakeholders: patients, physicians, hospitals, healthcare systems, and society.
Biomarkers avoiding excessive or detrimental antibiotic exposure
Studies and cost models have evaluated the budget impact of procalcitonin-guided antibiotic stewardship per patient, the reduction in the number of antibiotic resistance cases, and the cost per day of antibiotic consumption avoided. In a country like Belgium, this translates into savings of 1.98€ million, driven by a reduction of 666,868 antibiotic days 21.

Clinical decision support software
Antibiotic therapy decisions can be assisted by innovative clinical decision support software. More timely and appropriate therapy can translate into substantial savings via the reduction of the cost of antibiotic therapy [-5 to -70%], the duration of length of stay [-1.6 to -17%], and personnel 22 33, as well as better patient outcomes through reduced mortality.

Antibiotic susceptibility testing
Antibiotic susceptibility tests help identify which antibiotic(s) the bacterial infection will respond to and which ones it is resistant to. This, in turn, enables the physician to prescribe the appropriate medication to treat the patient and prevent misuse.

Subglottic Secretion Drainage
The use of special tubes can enable clinicians to manage subglottic secretion drainage (SSD), a technique that removes oral and/or gastric secretions containing bacterial pathogens, which may lead to serious complications, including Ventilator-Associated Pneumonia (VAP). Clinical investigations by Bouza et al. (2008) into the use of an edotracheal tube providing SSD found a 30% reduction in antibiotic use among the overall patient population, attributed to lower rates of VAP.

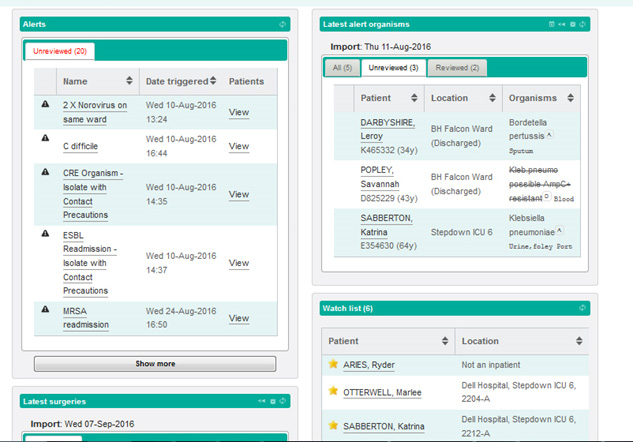
Clinical Surveillance Software
Surveillance systems play a key role in helping to conserve and steward the effectiveness of existing treatments, as well as supporting infection control practices by allowing clinicians to monitor infection scenarios and prescribe through the provision of bespoke triggers. By bringing together information from disparate sources, the system notifies practitioners of critical infection-related events, which aids clinicians in making targeted and timely interventions that prevent and control infections, and encourages the appropriate use of antibiotics to positively impact patient outcomes.
Resistance identification and reporting
When it comes to combating infectious organisms, microbial identification (ID) and antibiotic susceptibility testing (AST) are crucial for providing accurate information for targeted clinical responses and improved patient care outcomes. Manual and automated tools, including mass spectrometry, are complementary and ensure fast and accurate results for prescribing the right antibiotic at the right concentration to the right patient. Software has been developed to help hospitals in reporting and surveillance of resistance.

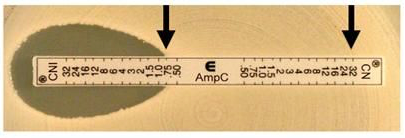
Identify emerging resistance patterns
ETESTs allow the detection and confirmation of resistant phenotypes for the most clinically relevant resistance mechanisms, including ESBLs (Extended-spectrum beta-lactamases), MBLs (Metallo-beta-lactamases) and AmpC beta-lactamases.
Outbreak management and surveillance
The more a hospital knows about the pathogens involved in an infection transmission or an outbreak, the better it can manage them. Services for Next Generation Sequencing-based genetic strain typing do exist that give extremely precise information about the disease agents suspected to be involved in infection transmission or HAI outbreaks. These powerful tools enable healthcare institutions and communities to make faster, better-targeted decisions, implement effective infection control measures, conduct more informed epidemiological investigations, reduce the incidence of future cases, and lower HAI-related healthcare management costs. Software tools are available for the surveillance of AMR at the hospital, regional, national and international levels.

Environment monitoring
Contaminated environmental surfaces are a significant source of pathogen transmission, including multi-resistant bacteria. These can cause severe infections, particularly in immunocompromised populations in hospitals.
Diagnostic tools can help to take control of the environment (including disinfection control).
Rapid surface testing technology enables the rapid and objective measurement of surface hygiene in under one minute. This technology helps measure, monitor and control hospital hygiene processes, enabling the delivery of continuous improvement in hygiene standards.

Wound care management
The World Health Organisation guidelines on the prevention of Surgical Site Infections (SSIs) suggest that the use of prophylactic Negative Pressure Wound Therapy (NPWT) may be used on high-risk patients for the purpose of preventing SSIs. Numerous studies in multiple surgical specialisations have been published, demonstrating the clinical and cost-effectiveness of NPWT for closed incision wounds following surgery. Cooper et al 2022) demonstrated a few surgical site complications (3.4% vs 13.3%; P=0.0013) and patients required fewer surgical (0.7% vs 4.8%; P=0.0666) and non-surgical (2.7% vs 12.9%; P=0.0017) interventions compared to those with standard of care. Respective total per-patient cost for the NPWT $1,047 compared to $2,036 for SOC in patients undergoing revision total knee arthroplasty. A further study by Svensson-Bjork et al. compared NPWT vs standard dressing after open inguinal vascular surgery and considered NPWT to be cost-effective over standard dressings due to the reduced SSI incidence (11.9% vs 30.8%; p=0.015) at no higher costs.

Medication monitoring
The appropriate use of antibiotics can be enabled at home through e-health, m-health, and other drug monitoring technologies. Misuse and non-adherence to antibiotic prescriptions are one of the key causes of the development of resistance.

- OECD (2023), Embracing a One Health Framework to Fight Antimicrobial Resistance. OECD Health Policy Studies, OECD Publishing
- European Centre for Disease Prevention and Control (2008). Annual epidemiological report on communicable diseases in Europe 2008. Report on the state of communicable diseases in the EU and EEA/EFTA countries
- Global leader’s group on AMR 2024
- ECDC. Antimicrobial consumption in the EU/EEA (ESAC-Net) Annual Epidemiological Report for 2023.
- Cost-effectiveness of screening, decolonisation and isolation strategies for carbapenem-resistant Enterobacterales and methicillin-resistant Staphylococcus aureus infections in hospitals: a sex-stratified mathematical modelling study; Kasim Allel, Patricia Garcia, Anne Peters, Jose Munita, Eduardo A. Undurraga, Laith Yakob The Lancet Regional Health – Americas, Volume 43, March 2025, 101019
- Tolley A et al. J Antimicrob Chemother 2024
- Scandret K et al. [B] Evidence review for rapid tests to inform triage and antibiotic prescribing decisions. NICE guideline NG237 2023; Smedemark SA et al. Cochrane Database of Systematic Reviews 2022; Zhang K et al. J Thorac Dis 2022; O’Brien et al. EUnetHTA Project ID: OTCA012. 2019; Verbakel et al. BMJ Open 2019
- Maltezou, H.C. et al., 2008
- NICE Evidence Review 2023
- Kardas-Sloma 2022
- Clark 2023
- Posnakoglou 2022
- Sundelin 2023
- Thomas EJ, Studdert DM, Burstin HR et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 2000; 38 (3): 261–271.
- Ayliffe GA. Role of the environment of the operating suite in surgical wound infection. Rev Infect Dis. 1991 Sep-Oct;13 Suppl 10:S800-4. doi: 10.1093/clinids/13.supplement_10.s800. PMID: 1754788.
- Umscheid, CA, Mitchell, MD, Doshi, JA, Agarwal, R, Williams, K, Brennan, PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011 Feb;32(2):101-14.
- Recommendations | Plus Sutures for preventing surgical site infection | Guidance | NICE
- Zucconi 2022
- Bejko 2015
- Pliakos 2018, Yo 2022
- Garnfelt 2023
- Nault 2017
- Laka 2020